FODMAPS & IBS
Irritable bowel syndrome (IBS) is one of the most common gastrointestinal disorders, affecting 10-20% of the population. (1) It is a benign but troublesome condition featuring symptoms such as (1, 2)
- Diarrhoea
- Constipation
- Abdominal Bloating
- Abdominal Pain or Discomfort
- Excess Wind
These symptoms fluctuate in severity from day to day, making it a turbulent condition. (3) IBS is a chronic condition and has to date no known etiology or cure. (2, 4) Genetics appear to play a role in susceptibility to IBS. (2) The high prevalence makes this condition a major contributor to reduced quality of life, work absenteeism and impaired social functioning. (4)
Screening, Tests & Diagnosis
If IBS is suspected, it is important that a physician rule out other conditions, such as coeliac disease, ulcerative colitis, food chemical sensitivity, gastrointestinal infections, endometriosis and ovarian cancer that can mimic IBS symptoms (3) These other conditions will be managed very differently to IBS.
IBS is diagnosed using the ‘Rome III’ criteria if an individual has suffered symptoms of a functional gut disorder for at least six months and have experienced for at least three months of the year: (4-6)
- Changes in bowel habits (diarrhea, constipation)
- Abdominal pain/discomfort
- Abdominal bloating/distention
A hydrogen and/or methane breath test will be completed to determine malabsorption of fructose, lactose and/or sorbitol. (5, 7) Although some of the gas produced in the large bowel is passed out as flatus, most of it transfers across the lining of the large bowel and into the blood stream where it dissolves into the blood. (3) Blood is carried to the lungs, and the gas is breathed out via the lungs (3) The results of this test will determine the modifications required in an individuals diet.
FODMAPS
Symptoms of IBS are most commonly triggered by a food intolerance; therefore dietary modifications have emerged as the first-line treatment. (2) Dietary therapy, in particular the low FODMAP diet has now developed as an evidence-based approach to managing IBS symptoms, effective in 75% of the IBS population. (2, 4, 5) FODMAPs are short chain carbohydrates that are poorly absorbed in the small intestine, are rapidly fermented by bacteria and create gas, and have a high osmotic effect, drawing fluid into the gut. (5, 7)
The FODMAPs acronym:
Fermentable
Oligosaccharides (fructans & galacto-oligosaccharides/GOS)
Disaccharides (lactose)
Monosaccharides (fructose in excess of glucose)
And
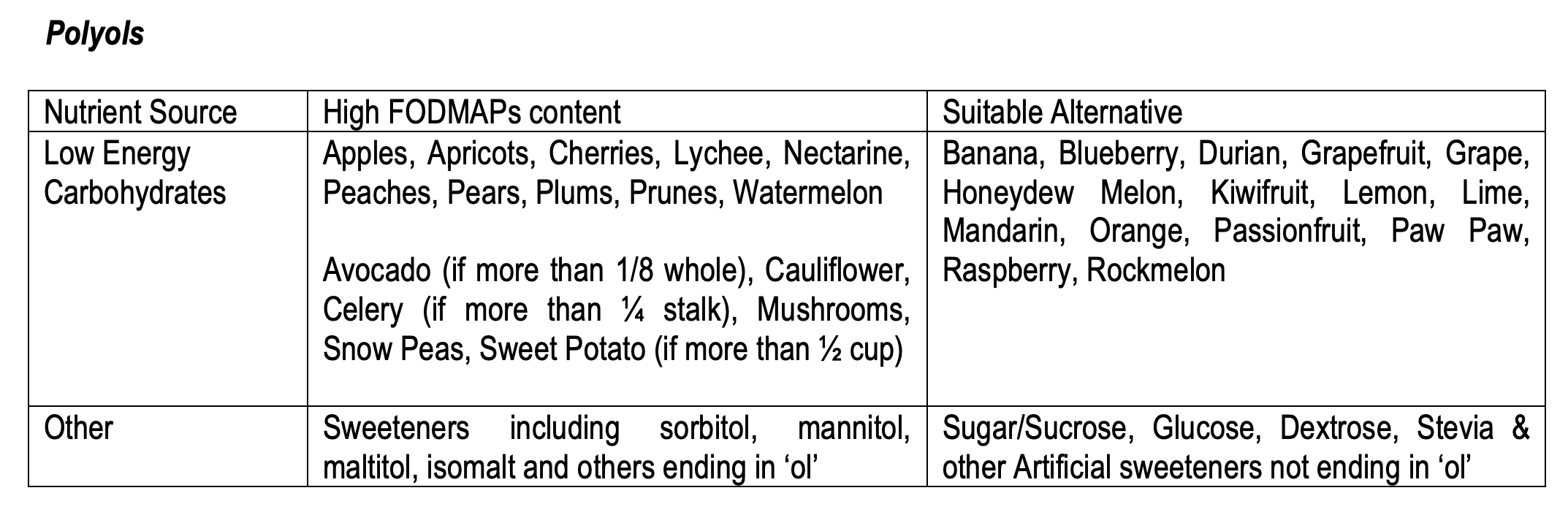
Polyols (eg. sorbitol, mannitol, xylitol, maltitol)
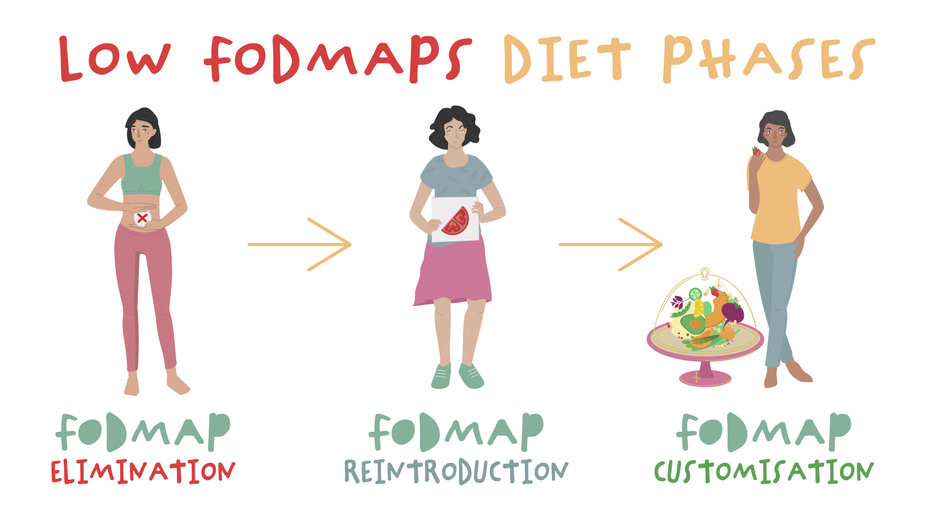
FODMAPs Dietary Intervention
Generally it is either a dietitian or gastroenterologist that will recommend a low FODMAP individualised diet for 6-8 weeks until they are symptom free. They would then guide their client through a FODMAP challenge, where foods are reintroduced strategically to determine the FODMAP intolerance. This often takes at least 6-8 weeks. It is important any FODMAP challenge is undertaken with the guidance of a health professional to avoid unnecessary elimination of foods in the diet long term.
Generally, all individuals diagnosed with IBS are advised by health professionals to avoid high fructan, GOS and mannitol containing foods. (2, 8) Further dietary modifications will be made to lactose, fructose and sorbitol only if indicated by the breath test. (2, 7) Each individual that has gone through this diagnosis and dietary prescription process will be given resources with detailed information on which foods to avoid or limit in their diet. The Monash University App is a popular resource, which is updated as new information is released.
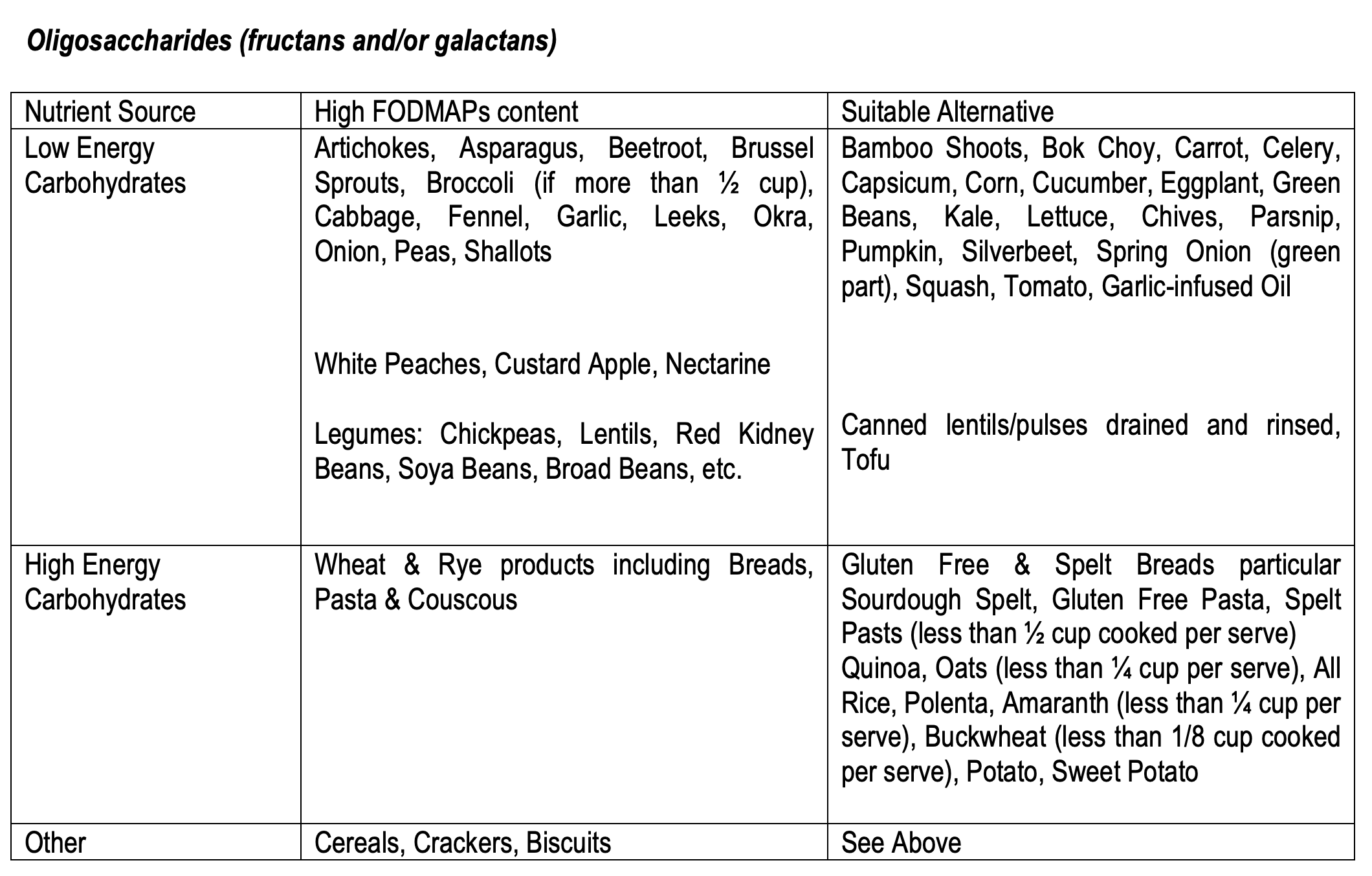
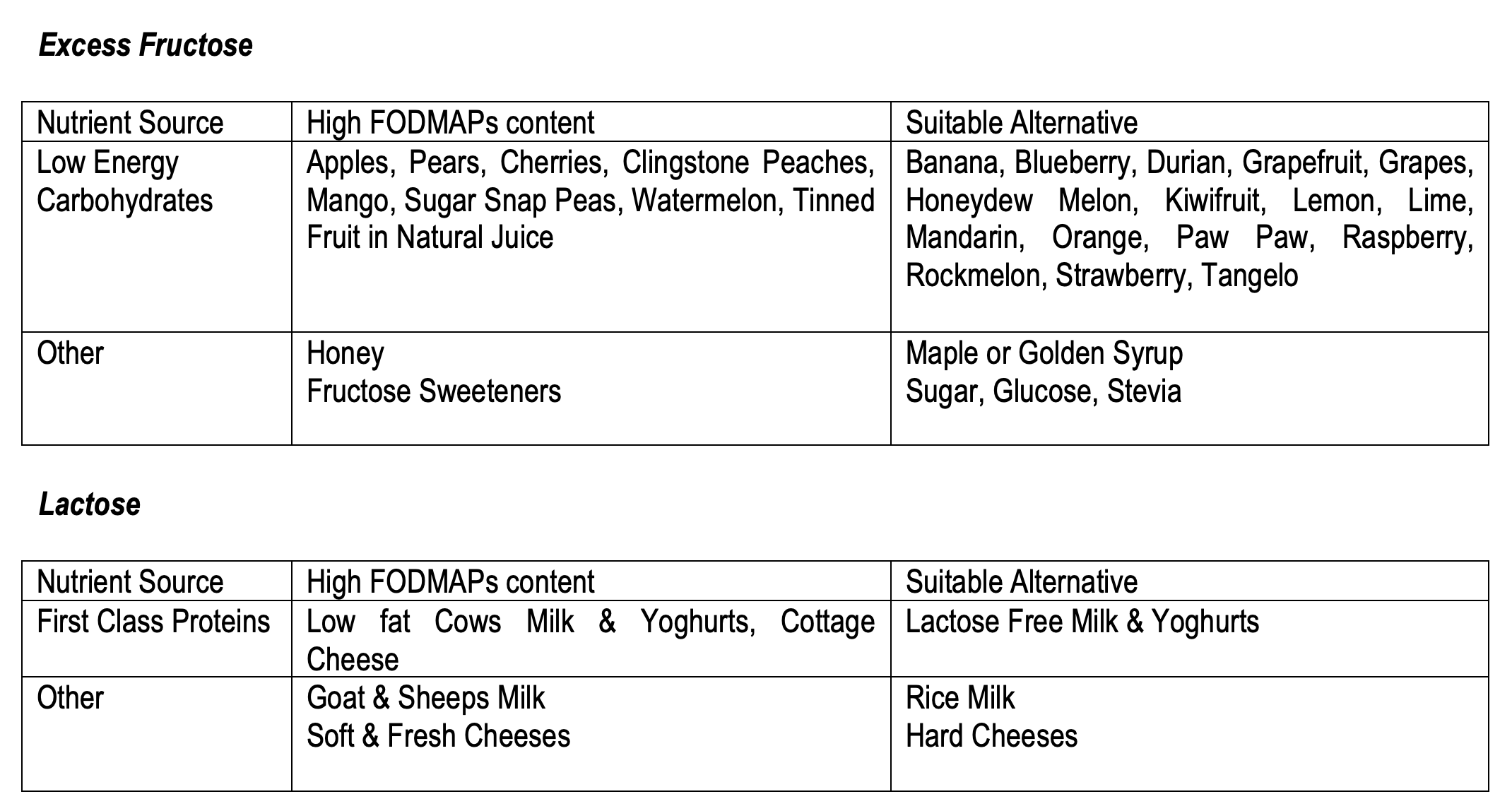
In our tables below, foods high in FODMAP content are highlighted utilising the macronutrient categories – low and high-energy carbohydrates, first class proteins, and ‘other’ to indicate discretionary choices. It is important to note that this is an evolving area, with the discovery of additional high & low FODMAP foods each week. Monash University currently has full time food technologists dedicated to analysing FODMAP content in their laboratory.
Helpful hints
- Fast absorbing carbohydrates including Glucose, Maltose, Maltodextrin, Sucrose, Gatorade, Powerade and other similar sports drinks are generally well tolerated.
- Nuts are generally low in FODMAPs, with the exception of Almonds, Pistachio and Cashews, which contain oligosaccharides. A small quantity, around 10 almonds is deemed a ‘safe’ level to avoid symptoms, and remains within suggested serving sizes in the TCB recipes.
- When increasing fruit, vegetable and overall fibre intake, individuals can experience similar symptoms to IBS such as excessive wind, and abdominal distension. Sulphur containing foods such as cruciferous vegetables, protein-rich meats, nuts and eggs, in particular egg whites can contribute to odorous gas.

- Drink plenty of water and avoid excessive soft drink consumption. Soft drink can contribute to gas, and will provide no nutritional benefit.
- Sports drinks and carb formulations that are based on Fractionated Barley Amylopectin, may not be tolerated well in individuals with IBS. Appropriate alternative fast acting carbohydrates include dextrose or glucose sports drinks.
- Latest research by Monash University indicates there are ‘safe’ levels of many of these foods. Therefore, individuals with IBS sufferers may find they can enjoy some of the high FODMAP foods in small or moderate amounts. For example, broccoli is deemed ‘safe’ if half a cup or less is consumed in one sitting.
- In terms of Protein supplements, lactose free are most suitable. Notes: high quality Whey Protein (80%+ protein) are often lactose free. Read the label carefully.
- Liquid Meals can be made with water, soy milk or almond milk instead of cows milk if lactose intolerance is indicated.
Practical Hints for better eating
Many of the recipes found in the transformationcookbook.com require very simple modifications to be appropriate for an individual with IBS. Often, removing or modifying the amount of onion consumed in a meal is all that is required to become FODMAP friendly. We use garlic and onion in many recipes to add flavour, so lack of flavour can be a common complaint with individuals following this diet. Some FODMAP friendly hints to flavour food include:
- Use the green part only from spring onions
- Fresh herbs including basil, coriander, parsley, rosemary, thyme
- Sprinkle of rock salt
- Use spices including turmeric, paprika, cinnamon, cumin
- Garlic Infused Olive Oil
- The ‘Must Have’ MP secret dressing! Simply omit the honey and garlic. It’s still delicious!
Transformationcookbook recipes can easily be modified depending on the intolerance. Use the appropriate substitutions in the tables above and consult your health professional.
An example a TCB Low FODMAP Meal Plan:
Meal 1 The 3 min Omlette
Meal 2 Mocha almondo cream – dairy free!
Meal 3 Healthy Chinese takeaway chicken – just omit onions
Meal 4 Rainbow muffin – simply omit onions
Meal 5 TCB Roast
Dessert: TCB Cobbler – just replace the peach with pawpaw or melon

Physical Activity
Physically active individuals with IBS will face less symptoms, and symptom deterioration than those that are physically inactive. (9) It has been proposed that this is due to the stimulation and increased gastrointestinal motility when physical activity is undertaken. (9) In turn, colonic transit time is improved (less constipation), gas and bloating is reduced. (9, 10) Endurance athletes however often experience adverse effects such as prompting an urge to defecate, diarrhoea and gastrointestinal cramps. (9) As per the broader population, incorporating resistance training and vigorous cardio exercise are fantastic ‘doses’ of physical activity for successful primary treatment in IBS.
Referral
It is important to refer to a physician immediately for further investigation if an individual experiences: (11)
- Blood in stools
- Nocturnal bowel motions
- Awakening by gastrointestinal symptoms
- Unintentional weight loss
- Has recently used antibiotics
- Symptom onset after the age of 50
- Symptoms with a family history of colon/bowel cancer.
It appears that eating a healthy Western breakfast’ of milk with high-fibre cereals, whole grain bread with honey, washed down with apple juice, is perhaps the worst way to start off the day for an adult IBS patient, utilising the transformationcookbook.com meal planner for hundreds of breakfast substitutions to help manage symptoms of IBS! (12)

References
1. Reza Ghadir M, Hossein Ghanooni A. Review of Pathophysiology and Diagnosis of Irritable Bowel Syndrome. Qom University of Medical Sciences Journal. 2014:1-4.
2. Shepherd SG, Peter. Food Intolerance Management Plan. Melbourne: Pengiun Group; 2011.
3. Shepherd S. Low FODMAP Recipes. Melbourne: Penguin Group; 2013.
4. Halmos EP, Power VA, Shepherd SJ, Gibson PR, Muir JG. A diet low in FODMAPs reduces symptoms of irritable bowel syndrome. Gastroenterology. 2014;146(1):67-75.e5.
5. Gibson PR, Shepherd SJ. Evidence-based dietary management of functional gastrointestinal symptoms: The FODMAP approach. Journal of Gastroenterology & Hepatology. 2010;25(2):252-8.
6. Lomangino K. The low-FODMAP diet: a new treatment approach for irritable bowel syndrome. Clinical Nutrition Insight. 2012;38(6):1-4.
7. Shepherd SJ, Gibson PR. Fructose malabsorption and symptoms of irritable bowel syndrome: guidelines for effective dietary management. Journal Of The American Dietetic Association. 2006;106(10):1631-9.
8. Muir JG, Shepherd SJ, Rosella O, Rose R, Barrett JS, Gibson PR. Fructan and free fructose content of common Australian vegetables and fruit. Journal Of Agricultural And Food Chemistry. 2007;55(16):6619-27.
9. Johannesson E, Simrén M, Strid H, Bajor A, Sadik R. Physical activity improves symptoms in irritable bowel syndrome: a randomized controlled trial. The American Journal Of Gastroenterology. 2011;106(5):915-22.
10. Lewis SJ, Heaton KW. Stool Form Scale as a Useful Guide to Intestinal Transit Time. Scandinavian Journal of Gastroenterology. 1997;32(9):920-4.
11. Whitehead WE, Palsson OS, Feld AD, Levy RL, Von Korff M, Turner MJ, et al. Utility of red flag symptom exclusions in the diagnosis of irritable bowel syndrome. Alimentary Pharmacology & Therapeutics. 2006;24(1):137-46.
12. Gwee K-A. Fiber, FODMAPs, flora, flatulence, and the functional bowel disorders. Journal of Gastroenterology & Hepatology. 2010;25(8):1335-6.